When food is scarce, stress hormones direct the immune system to operate in “low power” mode to preserve immune function while conserving energy, according to researchers at Weill Cornell Medicine. This reconfiguration is crucial to combating infections amid food insecurity.
“Both famine and infectious disease have been with us throughout our evolutionary history and often occurred at the same time. Yet little is known about how nutrition affects the immune system,” said senior author Dr. Nicholas Collins, an assistant professor of immunology, and a member of the Jill Roberts Institute for Research in Inflammatory Bowel Disease and the Friedman Center for Nutrition at Weill Cornell.

Dr. Nicholas Collins
The answer could be important in helping the 47 million Americans who are food insecure and face the risk of infectious diseases every day. “Mounting an immune response against infections requires a lot of energy. We have discovered a coordinated system that upholds immune function by shifting the composition and metabolism of immune cells,” Dr. Collins said.
The results, published Feb. 10 in Immunity, found that mice on a calorie-restricted diet fought off infection as well as mice that were fully fed, but did so while using very little glucose. This was possible thanks to glucocorticoids, stress hormones known for their role in regulating blood glucose. The researchers determined that glucocorticoids acted like master conductors, reorganizing immune cells and their energy usage to provide a survival advantage.
The research was co-led by Luisa Menezes-Silva, a visiting graduate student from the University of São Paulo, Brazil; Dr. Mingeum Jeong, a postdoctoral associate; and Dr. Seong-Ji Han, a research associate, all in the Collins lab at Weill Cornell.
Shifting Priorities
To understand the complex interactions involved in an immune response during scarcity, Dr. Collins and his team put mice on a 50% restricted-calorie diet and then exposed the animals to bacteria that infect the gut. The mice that were fed a standard diet experienced a metabolic crash— their blood glucose levels and body weight plummeted.
The researchers had expected this would happen to all the animals because mounting an immune response can consume up to 30% of the entire body’s fuel reserves. But in the calorie-restricted mice, the immune system appeared to be functioning perfectly well without using much glucose.
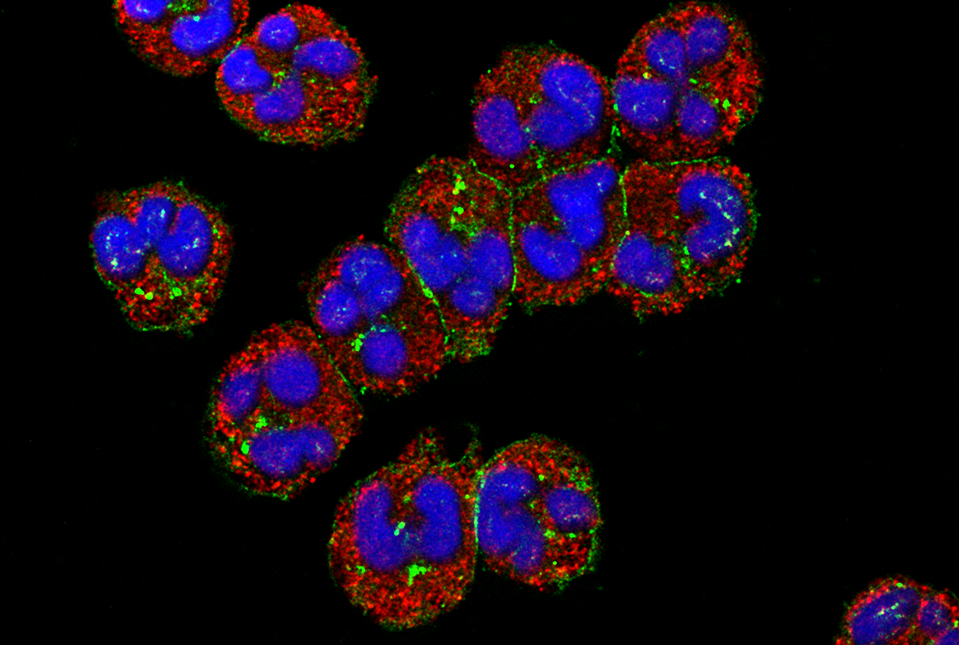
To unravel this enigma, the researchers inventoried the immune cells of the infected animals and discovered that T cells, which normally target invading microbes, were depleted in the calorie-restricted mice. Instead, short-lived neutrophils, which serve as the body’s first responders to infection, were ramped up to twice the normal amount and had measurably enhanced pathogen-killing abilities. The cells seemed to be operating in energy-saving mode, consuming much less glucose than neutrophils from well-fed animals.
“So, this hormone rewires the immune system to eliminate the infection while keeping blood sugar from dropping, which rescues the calorie-restricted animals from malnutrition,” said Dr. Collins.
Stress Hormones Lead the Charge
The researchers are breaking new ground by outlining how a sudden fall in food intake triggers glucocorticoid levels to rise, resulting in two major shifts. First, the body repositions certain immune cells—especially naïve T cells—into the bone marrow, which becomes a kind of “safe house” for when the cells are needed. Second, during an infection, glucocorticoids tilt the immune response away from energy‑intensive T cells toward neutrophils, abundant cells that act as immediate, short-lived defenders.

Pictured from left to right: Dr. Nicholas Collins, Dr. Seong-Ji Han, Dr. Mingeum Jeong and graduate student Luisa Menezes-Silva.
Beyond clearing a current infection, glucocorticoids prepare the immune system for repeat encounters with infectious agents. While the hormones direct killer T cells to stand down and neutrophils to step up, they also ensure memory T cells are preserved for future confrontations.
“Glucocorticoids reduce the immune cells that use up the most energy, while saving those that are critical for protection against future infections,” Dr. Collins said. “So, these hormones are involved in every step of the infection-fighting process.”
“Since glucocorticoids are induced not only by nutrient restriction but also by any form of stress, our findings might have broader applicability,” said Dr. Collins.
In the meantime, he and his team plan to explore what causes the system to fail when the degree and duration of calorie restriction are more severe. “We looked at reduced food intake over three weeks,” he said. “But when you cross the threshold into malnutrition, the whole system breaks down.” Understanding this collapse could inform better strategies to prevent infectious disease and infection-driven malnutrition in vulnerable populations.
This research was supported by the National Institutes of Health: grant R01AI182043 (NIAID), R00CA252443 (NCI), R00CA252443-03S1 (Office of Dietary Supplements), DK126871, AI151599, AI095466, AI095608, AI142213, AR070116, AI172027 and DK132244. Additional funding was provided by The Feldstein Medical Foundation, The Charles Frueauff Foundation, The Parker Institute for Cancer Immunology, the São Paulo Research Foundation (FAPESP #2023/01164-9 and FAPESP #2023/07482-2), the Cancer Research Institute Irvington Postdoctoral Fellowship (CRI12557), the Allen Discovery Center program, the Paul G. Allen Family Foundation, Cure for IBD, the Sanders Family and the Rosanne H. Silbermann Foundation.